Original Publication: 11/05/2019 – National Institutes of Health
Each year, millions of people get influenza, or flu. During the 2017-2018 flu season, 959,000 people in the U.S. were hospitalized and 79,000 people died after catching the flu. The annual seasonal flu vaccine is currently the best way to protect against the viruses that cause flu.
The flu vaccine works by stimulating the body’s immune system to make protective antibodies against the influenza virus. It takes about two weeks after getting the seasonal flu vaccine for antibodies to develop in the body and provide protection against flu viruses.
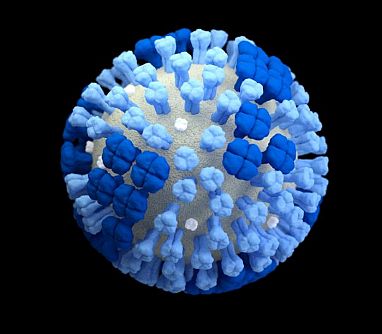
Most flu vaccines prompt the immune system to make antibodies against a protein found on the surface of the virus called hemagglutinin (HA). However, HA proteins mutate often as the flu virus evolves, requiring a new vaccine each year. Seasonal flu vaccines do not prevent all flu infections. Their effectiveness varies in part based on how well scientists predict the flu strains for that season.
Better vaccines are needed to provide broader flu protection against the multiple types and strains of flu that can cause flu outbreaks and possible pandemics. A research team led by Dr. Florian Krammer of the Icahn School of Medicine at Mount Sinai, Dr. Ian Wilson of Scripps Research, and Dr. Ali Ellebedy of Washington University School of Medicine set out to investigate new targets that could lead to a better flu vaccine. Their study was funded in part by the NIH’s National Institute of Allergy and Infectious Diseases (NIAID). Results appeared in Science on October 25, 2019.
The other surface protein on the flu virus is neuraminidase (NA). NA proteins change more slowly than HA proteins. Previous studies suggested that vaccines designed to target NA might offer broad protection against different virus strains and lessen the severity of illness. Tamiflu, the most widely used drug for severe flu infection, works by inactivating NA.
While studying the immune response to flu infection, the researchers noticed that one person with the flu seemed to be making antibodies against something other than HA. This person was infected with the H3N2-strain of influenza virus, and the sample was taken five days after symptoms had started. The team derived monoclonal antibodies (mAbs)—antibodies that bind to a single target—from the person and tested their ability to bind to different influenza proteins.
Three of the 45 mAbs tested bound to the NA protein of the H3N2 virus strain. Further testing revealed that these three mAbs also bound to NA proteins from several other types of flu virus. One of the mAbs, 1G01, bound all the viral NAs tested. All three mAbs targeted a region that’s similar among NA proteins and is critical for its function.
The team tested whether the antibodies could protect mammals against the flu. Mice were treated with the antibodies and then infected with several types of influenza A and B viruses. The antibodies were able to protect most of the mice from severe flu infections. When the viruses were tested in lethal doses, the 1G01 mAbs protected mice from death by any of them.
To determine whether the antibodies could also serve as a treatment, mice were given lethal doses of H3N2 influenza virus. They were then given low doses of the antibodies two to three days after being infected. All of the animals recovered after the treatment, demonstrating the therapeutic potential of these antibodies.
“Neuraminidase has been ignored as a vaccine target for a long time,” Ellebedy says. “These antibodies tell us that it should not have been overlooked. Now that we know what a broadly protective antibody to neuraminidase looks like, we could design novel influenza vaccines that are tailored to induce antibodies like these.”